Health Disparities and ACA: Where are we now? Where could we be?
The logical sequel to “where are we now?” is “where could we be?” in relation to the Patient Protection and Affordable Care Act (ACA). We must remember that there are (at least!) two sides to every policy issue. Ignoring the political debate about whether ACA has been successful for a moment, let’s consider how ACA is impacting marginalized groups, and how it could be useful in closing gaps in care for those same groups. Essentially, let’s address two simple questions – What are health and health care disparities? And how does the ACA impact disparities?
What are health and health care disparities?
For the sake of simplicity, we will define health disparities as a disproportionately higher burden of illness, injury, disability and/or mortality experienced by one population group relative to another group. Of course, disparities are not mere differences, but are instead a particular type of health difference closely linked with social and economic factors, systematic oppression and/or environmental disadvantage. Health care disparities are differences between groups in health insurance coverage, access to care, and quality of care. Ok, so what does this have to do with ACA?
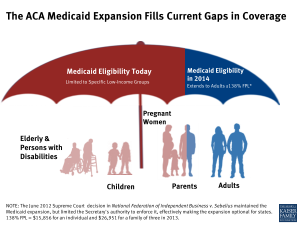
Not so fast. While ACA is a national policy, Medicaid, the primary government-funded insurance program to provide health care to low-income individuals and vulnerable groups is state-run or managed by cooperative agreements between the federal and state government. Recall also that in 2012 the Supreme Court decided that while the Medicaid coverage expansion would be maintained, the Secretary would be limited in authority to enforce the expansion (in National Federation of Independent Business v. Sebelius), effectively making the expansion optional for states.
How does the ACA impact disparities?
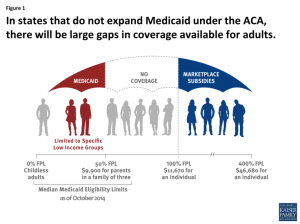 In a nutshell, states are not required to expand Medicaid benefits, leaving those who would be “covered” well, holding an umbrella with a giant hole in it. In fact, as of August 2014, 28 states including the District of Columbia were expanding Medicaid to provide additional benefits and services; however, 21 states were not and 2 were undecided. It also just so happens that a sizable number of states not moving forward with Medicaid expansions at this time are also states located in the South, among the poorest states and home to large percentages (~50%+) of communities of color. States in the South and largely rural states also serve more older adults, have more Medicaid/Medicare patients and maintain the highest rates of chronic health burden.
In a nutshell, states are not required to expand Medicaid benefits, leaving those who would be “covered” well, holding an umbrella with a giant hole in it. In fact, as of August 2014, 28 states including the District of Columbia were expanding Medicaid to provide additional benefits and services; however, 21 states were not and 2 were undecided. It also just so happens that a sizable number of states not moving forward with Medicaid expansions at this time are also states located in the South, among the poorest states and home to large percentages (~50%+) of communities of color. States in the South and largely rural states also serve more older adults, have more Medicaid/Medicare patients and maintain the highest rates of chronic health burden.
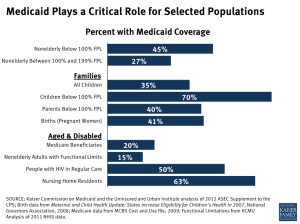
Not the warm-fuzzy you were expecting? Well, I did say that there was hope, no? “Where could we be?” is the pressing question that will continue to shape our health care system as we think of new ways to deliver care. The beautiful thing about state-run Medicaid programs is that states have some autonomy, at least in those opting to expand Medicaid, to actually address change at the SYSTEM level. In New York State for example, a primary goal is to “break the mold” of the current Medicaid program to offer innovative new ways of delivering a mix of services to improve population health. Streamlining emergency Medicaid processes, developing new ways to provide supportive housing and providing competency training to the NYS healthcare workforce are just a few ways New York is taking on service integration and system reform. One can only hope that such innovation, especially as it relates to training the health care workforce, follows a structural competency model to highlight the underlying root of health inequalities and how we, as health professionals, can change them.
It is an exciting time to be engaged in Medicaid redesign as policy makers and public health researchers are actually thinking through and talking to one another about how to offer more community services for those caught in the gap and how to meet people in need where they are. System change is indeed a beautiful thing. It will be an interesting experiment to observe how it all plays out and what the changes associated with ACA will bring in the years to come.